Diabetic Foot Ulcers

The main cause of foot ulcers in diabetic patients is often minor injuries happening when they cannot feel their feet properly. This happens due to a condition called peripheral sensory neuropathy. In simpler terms, it means their nerves do not work well, making them less sensitive to pain or injuries. Along with this, deformities in the foot shape and occasional trauma can play a role in causing foot ulcers. Additional factors in foot ulcer formation include calluses, swelling, and problems with blood circulation to the lower legs and feet. Neuropathy seems to involve various chemical processes and high blood sugar levels. Controlling blood sugar is vital in preventing neuropathy and foot ulcers. If you have diabetes and are experiencing foot ulcers, it is strongly suggested that you visit a podiatrist for immediate care.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with the foot specialists from Spartan Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in Battle Creek, and Marshall, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
What Causes Morton’s Neuroma?

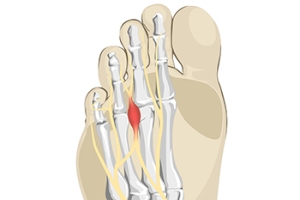
Morton's neuroma is a painful condition that affects the ball of the foot, typically between the third and fourth toes. It is caused by the thickening or enlargement of the tissue around a nerve leading to the toes. Several factors contribute to the development of Morton's neuroma. Wearing tight, narrow, or high-heeled shoes can compress the toes and increase pressure on the nerve, leading to irritation and inflammation. Additionally, individuals with certain foot deformities, such as high arches or flat feet, are more prone to developing Morton's neuroma because these conditions can alter the distribution of weight and pressure on the nerves. Engaging in activities that involve repetitive stress on the forefoot, like running or activities that require tight footwear, can contribute to the development of this condition. A foot injury or trauma can lead to the formation of scar tissue around the nerve, which can then become irritated and inflamed. If you experience symptoms associated with Morton's neuroma, such as pain, numbness, or a burning sensation in the ball of your foot, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact the foot specialists of Spartan Podiatry. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Battle Creek, and Marshall, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
The Importance of Addressing Foot Pain

Foot pain, though often dismissed as a temporary inconvenience, should never be ignored, as it can signify underlying issues that demand attention. Our feet, the foundation of our mobility, are intricate structures comprising bones, joints, muscles, and ligaments. Persistent pain may indicate conditions such as plantar fasciitis, arthritis, or tendinitis, which can worsen without intervention. Ignoring foot pain can lead to altered gait patterns, placing undue stress on other joints and potentially causing a domino effect of discomfort. Moreover, certain foot pain could be a symptom of systemic conditions like diabetes or circulatory issues, requiring timely medical intervention. Chronic foot pain may impact one's quality of life, hindering daily activities and diminishing overall well-being. By recognizing the significance of foot pain and seeking professional evaluation, individuals can safeguard the essential role their feet play in maintaining an active and healthy lifestyle. If you have any type of foot pain, it is suggested that you are under the care of a podiatrist who can provide you with effective relief methods.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with the foot specialists from Spartan Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Battle Creek, and Marshall, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
Problematic Diabetic Foot Symptoms

For those individuals with diabetes, about half experience nerve damage, often affecting the feet and legs. Numbness, tingling, or no symptoms at all may arise, depriving diabetic patients of pain perception. While the idea of pain-free living seems attractive, it heightens the risk of overlooking minor foot problems, such as cuts or sores, which can escalate and pose serious problems. The absence of pain sensation can lead to severe complications, potentially resulting in limb loss if wounds or ulcers on the foot do not heal. Factors increasing the likelihood of nerve damage include poorly managed blood sugar, prolonged diabetes duration, age over 40, excess weight, high blood pressure, and elevated cholesterol. Nerve damage, coupled with poor blood flow, significantly elevates the risk of foot ulcers that resist healing and may become infected. Daily foot checks are pivotal. Vigilantly examining your feet allows for early issue identification and timely treatment, crucial in reducing serious complications. A podiatrist is medically trained to manage foot problems associated with diabetes, including wound care for ulcers and infections. If you have diabetes, it is suggested that you schedule regular visits with a podiatrist to monitor the health of your feet.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact the foot specialists from Spartan Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Battle Creek, and Marshall, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Conditions
According to the American Diabetes Association (ADA), diabetes is a condition that affects approximately 23.6 million Americans. Around 750,000 new cases are diagnosed each year, and the disease’s most common form, Type 2 diabetes, makes up for 90 to 95 percent of these cases. Type 2 diabetes is especially prevalent among older Americans, those who are obese, and those who lead sedentary lifestyles.
Complications of the disease may lead to several foot and ankle-related conditions. The loss of nerve sensation, or neuropathy, can cause diabetics to lose feeling at the bottom of the feet and therefore leave them unaware of pain, pressure, and heat. Decreased circulation is another complication of diabetes that can slow down the healing of wounds and injuries; this can lead to the development of foot ulcers.
To prevent foot ulcers from forming, diabetics should examine their feet every day for small cuts and wear shoes that curtail pressure. Constant monitoring for the risk factors associated with ulcer formation can allow for early detection and therefore lessen the possibility of ulcers or, even worse, amputation. The removal of calluses and ingrown toenails should be left to the podiatrist to avoid improper removal and possible infection.
Diabetic patients may also experience foot deformities due to complications in their feet, such as limited joint mobility, muscle atrophy, and decreased fat padding. These complications can increase pressure in certain areas of the foot, which in turn can cause certain deformities, such as hammertoe, to form. Another deformity, Charcot foot, develops due to the collapsing of microfractures in the bones of the feet. The resulting deformity is a foot that is flattened and wider in appearance.
To help minimize pressure and prevent the development of these diabetes-related foot and ankle conditions, your podiatrist may consider using orthotics or special shoes. Charcot foot may be treated using walkers, custom orthotic insoles, or non-weight-bearing or rigid weight-bearing casts or braces. In more serious cases, surgery may be considered to treat more developed deformities. Ulcers can be further cared for with the help of proper diet, medication to control glucose, intensive wound care, and infection treatment.